Is Non Diabetic Hypoglycemia Dangerous
Introduction
Yes, non-diabetic hypoglycemia can be dangerous. It is a condition in which a person’s blood sugar level drops too low. This can happen for a number of reasons, including certain medications, medical conditions, and malnutrition. Untreated hypoglycemia can lead to serious complications, including seizures, coma, and even death.
If you are experiencing any of the symptoms of hypoglycemia, it is important to see a doctor to get a diagnosis and treatment plan. With proper care, most people with non-diabetic hypoglycemia can live a normal life.
Hypoglycemia, a condition characterized by low blood sugar levels, can occur in individuals without diabetes. While it may not be as common as diabetic hypoglycemia, non-diabetic hypoglycemia can still pose significant health risks if left untreated. The severity of the condition and its potential consequences depend on the underlying cause and the individual’s overall health status.
The Body's Energy Source: Blood Sugar
Blood sugar, also known as glucose, serves as the body’s primary source of energy. It fuels cells throughout the body, enabling them to function optimally. When blood sugar levels drop below a certain threshold, the body experiences a state of hypoglycemia.
The Role of Insulin in Blood Sugar Regulation
Insulin, a hormone produced by the pancreas, plays a crucial role in regulating blood sugar levels. It acts as a key that unlocks the doors to cells, allowing glucose to enter and provide energy. In individuals with diabetes, the body’s ability to produce or use insulin effectively is impaired, leading to fluctuating blood sugar levels.
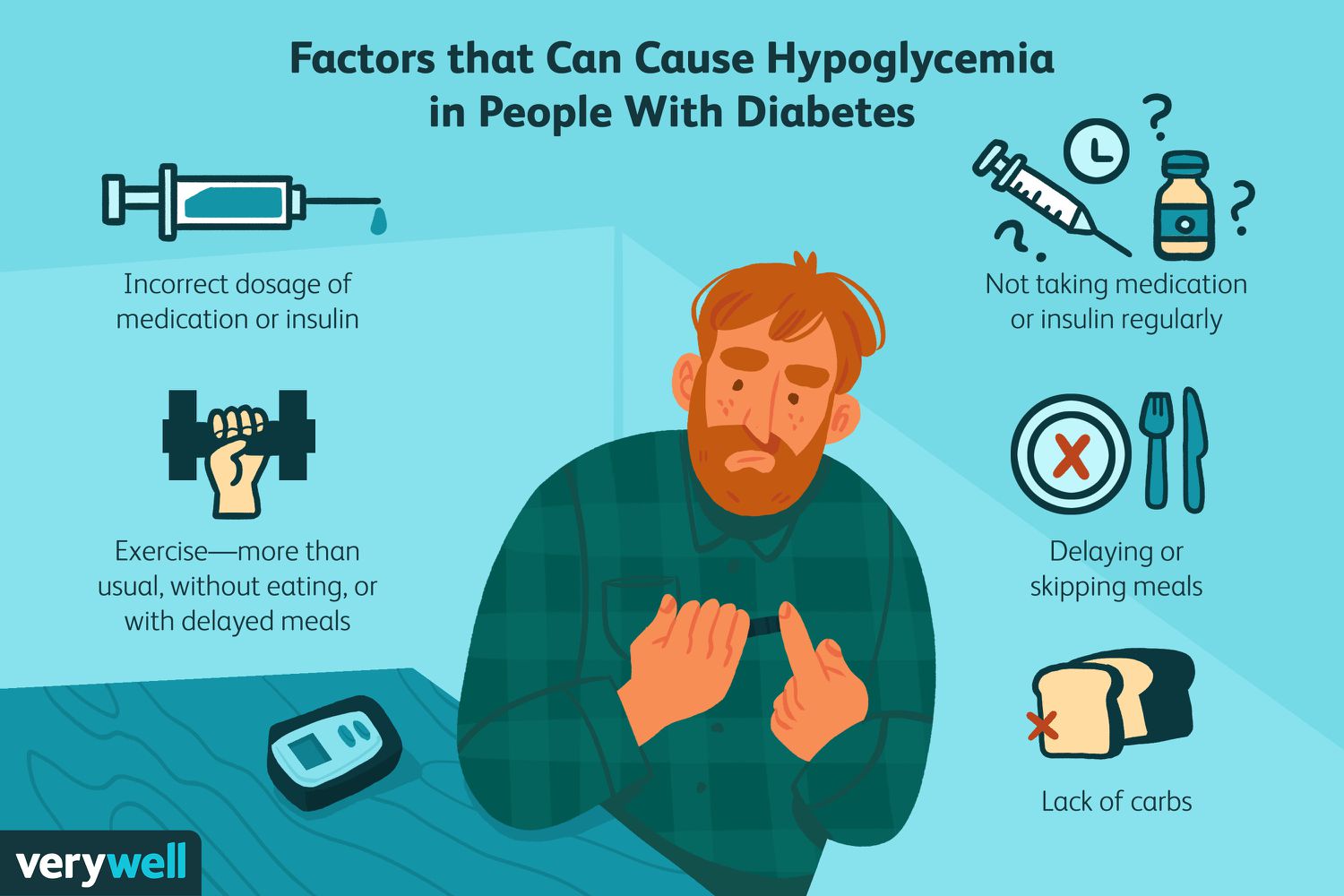
Causes Of Non Diabetic Hypoglycemia
Several factors can contribute to non-diabetic hypoglycemia. These include:
Medications: Certain medications, such as beta-blockers, sulfonylureas, and insulin, can cause blood sugar levels to drop too low.
Medical conditions: Hormone imbalances, liver disease, kidney disease, and certain genetic disorders can affect the body’s ability to regulate blood sugar levels.
Malnutrition: Severe malnutrition or eating disorders can lead to hypoglycemia due to insufficient fuel for the body’s cells.
Hypoglycemia Symptoms Without Diabetes
Here are some of the symptoms of non-diabetic hypoglycemia:
Shakiness
Sweating
Confusion
Irritability
Hunger
Rapid heartbeat
Headache
Blurred vision
Nausea
If you experience any of these symptoms, it is important to check your blood sugar level with a glucose meter. If your blood sugar level is below 70 milligrams per deciliter (mg/dL), you need to eat or drink something to raise it quickly.
Potential Complications
If left untreated, non-diabetic hypoglycemia can lead to serious complications, including:
Seizures: When blood sugar levels drop too low, the brain may not receive enough energy to function properly, leading to seizures.
Coma: In severe cases, hypoglycemia can cause a coma, a state of prolonged unconsciousness.
Brain damage: Chronic hypoglycemia can damage brain cells, potentially leading to cognitive impairments.
Death: In rare instances, untreated hypoglycemia can be fatal.
How To Treat Low Blood Sugar Without Diabetes
Fortunately, there are several measures that can help prevent non-diabetic hypoglycemia or manage it effectively:
Regular meals and snacks: Maintaining a consistent eating schedule helps maintain stable blood sugar levels.
Monitoring blood sugar levels: Regularly checking blood sugar levels can help identify early signs of hypoglycemia and allow for prompt intervention.
Carrying snacks: Keeping snacks readily available can help raise blood sugar levels quickly if needed.
Medication adjustments: Consulting with a doctor about medication dosages may be necessary to prevent hypoglycemia.
Addressing underlying conditions: Treating underlying medical conditions that contribute to hypoglycemia can help manage blood sugar levels.
Maintaining a healthy lifestyle: A balanced diet, regular exercise, and adequate sleep can support overall health and reduce the risk of hypoglycemia.
Diagnostic Test For Hypoglycemia
The Diagnostic Journey: Uncovering the Clues
The first step in diagnosing hypoglycemia involves a thorough medical history and a detailed account of the patient’s symptoms. The doctor will inquire about the frequency, severity, and timing of symptoms, such as shakiness, sweating, confusion, lightheadedness, and hunger. Additionally, the doctor will explore the patient’s dietary habits, medication regimen, and any recent changes in lifestyle or health conditions.
Blood Sugar Testing: The Gold Standard
If hypoglycemia is suspected, a blood test to measure blood sugar levels is the gold standard for diagnosis. A fasting blood sugar test, typically performed after eight hours of not eating, provides a baseline measurement. However, a random blood sugar test can be used if symptoms are present at the time of testing. A blood sugar level below 70 mg/dL (3.9 mmol/L) is generally considered hypoglycemia.
Individualized Thresholds: Understanding Personal Variations
It is important to note that individuals have varying baseline blood sugar levels, and the threshold for hypoglycemia can differ from person to person. Factors such as age, overall health, and certain medications can influence blood sugar levels. Therefore, the doctor will consider the patient’s individual circumstances when interpreting blood sugar test results.
Beyond Blood Sugar: Unveiling Underlying Causes
While blood sugar testing provides valuable information, additional tests may be necessary to determine the underlying cause of hypoglycemia. These tests may include:
Glucose tolerance test: This test measures how the body responds to glucose intake.
Hormone tests: These tests assess the function of the pancreas and other hormone-producing glands.
Imaging tests: Ultrasound or CT scans can be used to evaluate the pancreas and other organs that may contribute to hypoglycemia.
The Significance of Timely Intervention
Early diagnosis and prompt intervention are crucial for managing hypoglycemia and preventing its potential complications. By identifying the underlying cause and implementing appropriate treatment strategies, individuals can maintain stable blood sugar levels and minimize the risk of seizures, coma, brain damage, and even death.
Conclusion
In summary, non-diabetic hypoglycemia, while less common than diabetic hypoglycemia, can still pose significant health risks if not managed properly. By understanding the causes, symptoms, and potential complications of non-diabetic hypoglycemia, individuals can take preventive measures and seek timely treatment to avoid serious health consequences.